Polio-free India: It seemed impossible until it was done
Mar. 25, 2024
India’s journey from the world’s epicentre of a highly infectious viral disease to turning polio-free was like walking on eggshells: Every step we took mattered.
On 27 March 2014, India was officially certified wild poliovirus-free. This pivotal moment not only marked a triumph for the country itself, but for the whole world as it proved the biological and technical feasibility of polio eradication, it also paved the way for the entire WHO South-East Asia Region (SEARO) to be certified wild polio-free.
This year, 27 March marks the 10-year anniversary of this triumph, serving as a powerful reminder of the collective will and commitment that made overcoming a seemingly insurmountable health challenge possible.
I spent close to six enriching years of my life serving as the project manager of the National Polio Surveillance Project (NPSP) for WHO India. My work entailed providing technical assistance and strategic guidance to the national programme. I was also in charge of poliovirus surveillance, monitoring mass vaccination campaigns, crafting corrective measures and strategies, and working closely with government counterparts at all levels to ensure every child was vaccinated enough times to build their immunity. We delivered around 1 billion doses of polio vaccine to 172 million children each year over the course of four years leading up to the last case. And many more in the years after.

Taking a step back to reflect on this journey, there were several factors contributing to the monumental success of ending polio in India. The first fundamental factor was government commitment that consistently translated into diligent administrative action at the operational level. Even the district administrators were fully aligned with and committed to taking corrective measures based on evidence: accepting programmatic gaps and challenges and then committing to addressing them urgently.
The second, was the effective multi-actor system that allowed us as partners to provide technical assistance needed at the implementation level. We had the evidence: real-time data, including monitoring data, at the operational level that guided timely corrective actions. This data was put to good use – to recommend changes that the government took on board. I must emphasize both individuals’ and institutional willingness to make changes based on evidence mattered.
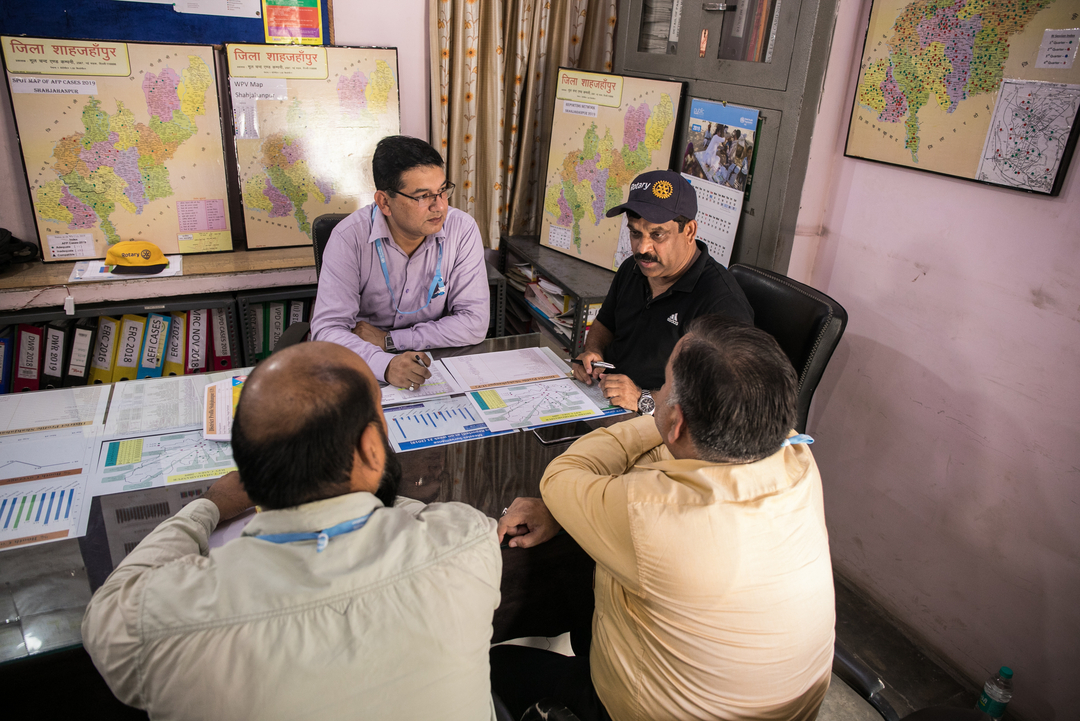
We also focused on the infrastructure that could appropriately manage community engagement and deploy the right community influencers, which led to collective action. In addition to this, an effective technical and managerial workforce on the ground was instrumental in making sure ideas turned into action. At the same time, the workforce was fine-tuned to meet the needs of the programme, which helped us as partners to work seamlessly together in our respective fields.
2011, the year when the last polio case was confirmed, was a year of great anxiety for us in India, but it was also the year of great effort to search for the virus. The more time that lapsed since the last confirmed wild poliovirus case, the higher the political stakes for any district or state to report a case of polio. And the media, in turn, began to set expectations that raised the stakes to match Mount Everest. It almost felt like we had held our breath while working away.
When we managed to end polio in India, this milestone was a major boost to public confidence in public health in the country, to the Ministry of Health, to every health worker, to caregivers, and to all our partners. Our efforts had paid off. The jubilation was just exceptional. The momentum had received a lot of support and enthusiasm within the ministers of health and the countries of the South-East Asia region, and this was very helpful for the polio programme on multiple fronts. We felt the dual sense of victory of humankind over one challenge, and regional and global solidarity and collective action of countries supporting and encouraging each other to eradicate polio in Nigeria, Afghanistan, and Pakistan.
I think the biggest learning of all of this would be that when entire countries and their leadership are working in unison, towards a shared vision of a healthier future for our children, a sense of mutual accountability is automatically established. All parties feel responsible for their own roles.
It was always a constant process of programme assessment and refinement.
And it seemed impossible until it was done. That’s how I feel today about the situation in Afghanistan and Pakistan, the two countries where polio is still endemic.
The path potholed with challenges is the same path laden with multiple opportunities that we need to seize. With the lowest ever level of wild poliovirus transmission, genetic diversity and the smallest geographical spread, we have a real window of opportunity to end polio. The efforts of our courageous health workers at the forefront, and the ongoing political commitment of leaders at all levels of the programme have brought us very close to our goal.
But we know there is more to be done if we are to prevent the virus from paralyzing another child ever again. This means, reaching every child with polio vaccines enough times to boost their immunity, using evidence from the field to adapt our programmatic approach, being willing to make changes, maintaining highly vigilant surveillance for poliovirus and, most importantly, making sure that everyone - from the highest political offices to the media, donors and the communities - works in concert to end polio, once and for all.
The persistent threat of the virus spreading and paralyzing children far across the globe is a warning that we must heed. It shows us that polioviruses are tenacious and thrive when children are under-immunized. It also serves as a reminder that we still need to constantly refine the programme in our relentless pursuit for children we have missed. This simply has to continue, even more so when we have a high level of control over the virus, so that complacency doesn’t steer us away from our path.
There are major programmatic shifts in play for both Afghanistan and Pakistan in 2024, particularly building on concerted efforts to zero-in on the virus through the risk categorization approach recommended by the Technical Advisory Group. We have it in our hands to once again achieve the impossible. As long as the virus exists, there is no room for error.
Once again, it feels like we are walking on eggshells. Every step we take matters.